An ultrasound to evaluate your baby’s growth
An ultrasound to evaluate your baby's growth
What is the ultrasound?
An ultrasound can provider evaluate your baby’s growth. An ultrasound is an imaging technique that uses sound waves to produce images of the fetus inside the womb. And can help your health care provider evaluate your baby’s growth and development and monitor your pregnancy. In some cases, a fetal ultrasound is used to evaluate potential problems or help confirm a diagnosis.
Why is a fetal ultrasound important during pregnancy?
An ultrasound to evaluate your baby’s growth ,It is one of the few ways your pregnancy care provider can see and hear your baby. It can help them determine how far along you are in pregnancy, if your baby is growing properly or if there are any potential problems with the pregnancy. its may occur at any time in pregnancy depending on what your provider is looking for.
What can be detected in a pregnancy ultrasound?
Generally prenatal ultrasound does two things:
- Evaluates the overall health, growth and development of the fetus.
- Detects certain complications and medical conditions related to pregnancy.
In most pregnancies, ultrasounds are positive experiences and pregnancy care providers don’t find any problems. However, there are times this isn’t the case and your provider detects birth disorders or other problems with the pregnancy.
Also Reasons why your provider performs a prenatal ultrasound are to:
- Confirm you’re pregnant.
- Check for ectopic pregnancy, molar pregnancy, miscarriage or other early pregnancy complications.
- Determine your baby’s gestational age and due date.
- Check your baby’s growth, movement and heart rate.
- Look for multiple babies (twins, triplets or more).
- Examine your pelvic organs like your uterus, ovaries and cervix.
- Examine how much amniotic fluid you have.
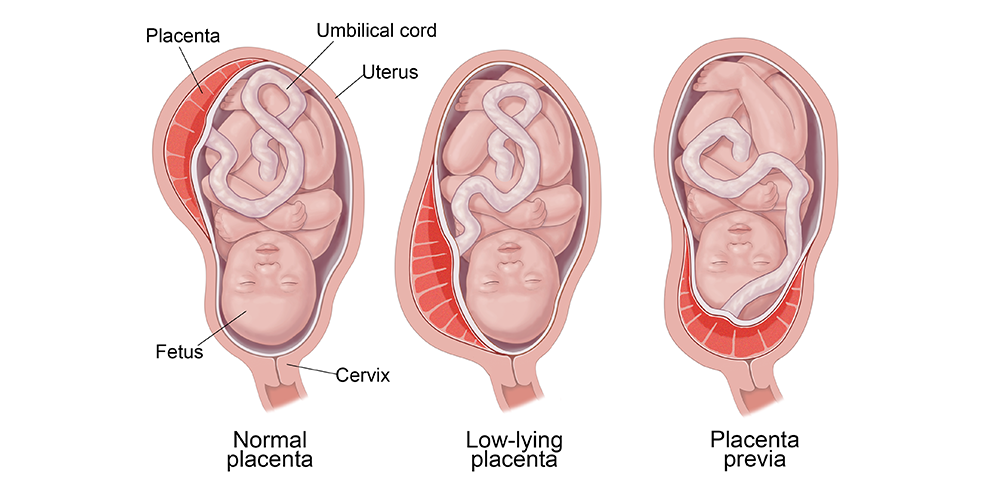
- Check the location of the placenta.
- Check your baby’s position in your uterus.
- Detect problems with your baby’s organs, muscles or bones.
Why is a fetal ultrasound important during pregnancy?
Also an important tool to help providers screen for congenital conditions (conditions your baby is born with). A screening is a type of test that determines if your baby is more likely to have a specific health condition. Your provider also uses ultrasound to guide the needle during certain diagnostic procedures in pregnancy like amniocentesis or CVS (chorionic villus sampling).
at the present time part of a biophysical profile (BPP), a test that combines ultrasound with a nonstress test to evaluate if your baby is getting enough oxygen.
 Fem Clinic
Fem ClinicHeliopolis: 94 El Merghany Street in front of the Girls College metro station
Fifth Settlement: Clinic 215, second floor, HCC building, behind the Air Hospital – New Cairo
For inquiries and reservations
 00201274777359
00201274777359Haitham_al-Tahawi #pregnancy #birth #microscopic injection #women’s health #breastfeeding #uterine #men_infertility #IVF #IVF #abortion #good morning #bahrain #egypt
An ultrasound to evaluate your baby’s growth Read More »